I think it strange and disheartening that as a society, once a friend or a loved one is diagnosed with Alzheimer’s, the overwhelming reaction is to feel primary sympathy for the spouse and family, rather than for those struck down. It seems that after the initial blow has been absorbed, we are very quick to diminish, and then sever, emotional connections with those losing their short term memory. For many of us, half a man, is no man at all.
Why is that? Why are we so quick to run? Because we feel helpless, or because we come to believe that our loved one is gone? And what impact does that aversion have on the care of those afflicted with Alzheimer’s?
It is as if we conclude that if Mom doesn’t recognize me, then I won’t recognize her. Perhaps this is why only about 15% of people living in dementia units receive regular visitors. As a culture, we are quick to saw the branch, even when we are standing on it.
It is of course a bitter and maddening challenge, as to what our model of care should look like for someone with dementia. Today we have two models: institutional care, and a more ambitious model consisting of a pharmacological regimen of memory saving drugs like Aricept and computer games such as Luminosity. Unfortunately, as Consumer Reports tells us, the memory saving drugs have little more benefit than placebos, and once we tire of the games, we give up. So we really have only one model of care: Institutional. This should be grossly unacceptable for Baby Boomers as we project our own future needs. In the next ten years, 2,000,000 more Americans will fall prey to Alzheimer’s, all of them Boomers, like me. So what should be done?
For any aging person, whether they have dementia or not, they continue to have a desire for purpose and resolution. Existential needs do not end because memory becomes blurry. And neither of these objectives can be achieved in stultifying isolation that currently prevails for those with dementia.
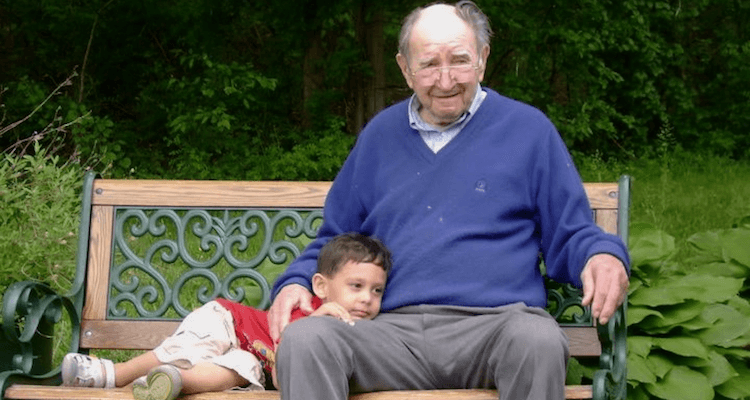
Purpose or meaning is of course a perplexing concept, but there is collective comfort in establishing ourselves in a context. Josiah Royce tells us in his 1908 book “The Philosophy of Loyalty”, that being merely fed and housed is often emotionally meaningless, and that we need a cause beyond ourselves. This can be a nation, tribe and most importantly, a family. Families, give us context, a legacy, an enduring purpose. I may know my days are numbered, but in the eyes of my children and grandchildren, the days of my family are not. But for the isolated Alzheimer’s victim living behind a Maginot Line, this lack of purposeful connection must be a horror.
Resolution, may be an even more compelling concern enmeshed in family relationships. Naomi Feil, the great pioneer in dementia care, tells us in” The Validation Breakthrough” that as we prepare to die, we have a need to resolve un-resolved memories, and relationships. Perhaps I was sexually abused as a child which was a memory suppressed, my husband was an alcoholic despite my lionization of him, or I was a terrible and vindictive mother, which was obvious to all but me. (No, obvious to me too.)
As we approach death, Feil suggests we want to heal, apologize on some level, and to be understood. We need resolution, and what she calls, validation. Again, none of this in conceivable if we are abandoned in a lock down unit of a nursing home.
So as families and friends run from what they think are dementia besotted ghosts of those they once loved, they are in fact depriving their loved ones of meaning and resolution, basic end of life human needs.
When we ask what a meaningful model of dementia care should look like for Baby Boomers, or how do we want to be cared for, it must contemplate, as it is for eons before, a family. And for those families that do remain engaged, please know, that you are quite literally doing, God’s work.